Depression is a widespread psychological condition, which impacts more than 300 million individuals globally, resulting in harmful effects like suicide.
Major depressive disorder (MDD) is a severe condition linked with multiple relapses and slow healing throughout episodes. Depression is a leading cause of impairment globally, and those experiencing psychotic episodes are at a greater risk of suicidal activities. Despite the availability of multiple psychopharmacological agents for managing depression, about 10-20 percent of patients hospitalized experience a recurrence of the condition following their initial rehabilitation.
Treatment-resistant depression
TRD impacts more than one percent of the population in the United States, and about 30 percent of all patients are stressed owing to symptoms that are immune to therapy. TRD results from severe psychosocial deficiency and low social /professional/ learning results. Treatment-resistant depression is defined by the inability to reply to at least two medications over four weeks at maximum dosage. Disease pathology is currently unclear.
The monoamine theory postulates that depressive symptoms are mainly triggered by the decrease in the supply of monoamines within nerve cells. Many antidepressant medications include using a monoamine neurotransmitter pathway (e.g., noradrenaline, dopamine, or serotonin). Therapeutic results of conventional antidepressant medications only begin to manifest after 4-12 weeks of therapy, meaning that pharmacological agents that deliver immediate antidepressant effects might be needed in clinical practice. To optimize the potency of a medication, clinicians must look to other goals outside monoamine structures.
Treatment-resistant depression lets you feel lost and frustrated. The symptoms sometimes return after months or years. After the effort it takes to seek help, someone can feel demoralized when they realize they are not improving.

Glutamate
Glutamate, the primary excitatory amino acid of the brain, has biochemical consequences. These functions involve synaptic growth and repair, cognitive control, regulation of other neurotransmitters and connectivity in the brain, and cell death (nerve cell damage or death). Glutamate processes have been involved in numerous diseases, including mood and anxiety, schizophrenia, and drug misuse, specifically alcohol. And from the stroke and severe brain damage, Alzheimer’s syndrome, and amyotrophic lateral sclerosis.
Glutamate is expelled from nerve cells, binds to receptors, and is brought back up by reuptake transporters. As diverse as the glutamate receptors are, some subtypes may be classified by their molecular and pharmacological properties. Glutamate receptors are classified into two major groups, ionotropic or metabotropic.
Ionotropic glutamate receptors
Ionotropic glutamate receptors are categorized into NMDA, AMPA, and kainate. Each subtype has several variants. The receptors’ model is divided into three types, with eight subtypes. Drugs of different glutamate receptor subtypes and various effects on glutamate activity (various physiological and clinical outcomes). The medicines that modulate glutamate activity through NMDA receptors are most clinically significant. However, there is also interest in traditional AMPA and metabotropic receptors.
More than 50 years ago, glutamate-modulating pharmaceutical treatment was first used to cure psychiatric illnesses. Cycloserine is a drug developed to combat tuberculosis. As given to suicidal patients with tuberculosis in a high dosage, in 1959, Crane confirmed that cycloserine aided in antidepressant results. But it was correlated with significant adverse effects, particularly in young people. Cycloserine is an amino acid derivative of alanine. It’s an antagonist at the NMDA receptor site in low levels, but it becomes a partial agonist in higher doses.
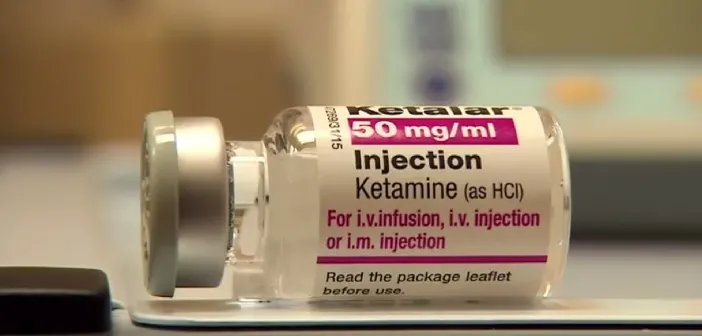
Role of Ketamine
Ketamine is an NMDA receptor that binds to µ and sigma receptors with strong affinity. Ketamine has been recorded to have the potential to modulate dopamine transmission, although it’s not clear if the function is connected to its antidepressant impact. Ketamine is effective in animal models of depression and is useful in human depression trials. Quick and persistent antidepressant results have been observed in various instances with Ketamine and in control trials.
Ketamine’s effect on suicidal ideation
Suicidal ideation is one of the worst psychologically troublesome to react to and involves most cases of suicide. Participants in the experiments were at higher risk for suicide, although they were included if they had “mild suicidal ideation.” Studies have also shown that there is a drop in SI after ketamine administration. In research evaluating the impact of Ketamine on suicidal ideation in persons with treatment-resistant depression, Ketamine decreased stress and suicidal ideation for two weeks following frequent infusions. In 14 patients with MDD admitted to the emergency room, a single 0.20 mg/kg dose of Ketamine administered over 1-2 min decreased [SI] dramatically when measured at 40 min post-infusion.
Analysis of suicidal patients with mood and anxiety problems treated in psychiatric clinics found a rapid decrease of suicidal ideation after Ketamine compared with midazolam. Change in researching the usage of Ketamine could contribute to its use in healthcare settings where emergency medicine is required. As a study into the anti-suicidal properties of Ketamine is still underway, it is impossible to evaluate the impact of Ketamine on suicide. However, further research is required on the neuroinflammatory mechanisms that connect suicidality and Ketamine’s therapeutic effect.
Effects on Anhedonia and Cognition
A study exploring the anti-suicidal properties of Ketamine discovered decreased depressive thinking and emotions that follow suicidal ideation following ketamine administration. A detailed analysis of clinical studies indicates that high pretreatment can be correlated with a higher reaction rate. Studies suggest that Ketamine’s antidepressant benefits can be associated with increased perceptual, social, and executive abilities (e.g., cognitive flexibility, memory, behavioral inhibition, planning). The prefrontal cortex neural networks help both changes in mood and enhancements in operation. Anhedonia progress was more highly associated with depression overall. This indicates that anhedonia’s improvement is pseudo-specific and not clinically relevant. It is due to the antidepressant effect.
The pleasure-reward function is directly linked to numerous psychiatric disorders and suicide. Ketamine stimulates the cingulate cortex, orbitofrontal cortex, hippocampus, and basal ganglia. Physicians should be aware of the association between agitation, anhedonia, SI, and cognitive deficiencies after IV ketamine.
Conclusion
In the end, an abundance of cumulative findings shows that Ketamine is an appropriate therapy for TRD patients. It has also been found beneficial for managing a bipolar patient, PTSD, and acute stress. In this stage, physicians and patients should consider the minimal literature on Ketamine prescribing and the dangers associated with long-term usage. However, we agree that Ketamine will become an essential aid in treating severe mood and anxiety disorders.


